Maximizing Value: The Hidden Benefits of Preventing Hospital-Acquired Pneumonia Through Oral Hygiene

Published by Infection Control Today
High Cost of Pneumonia
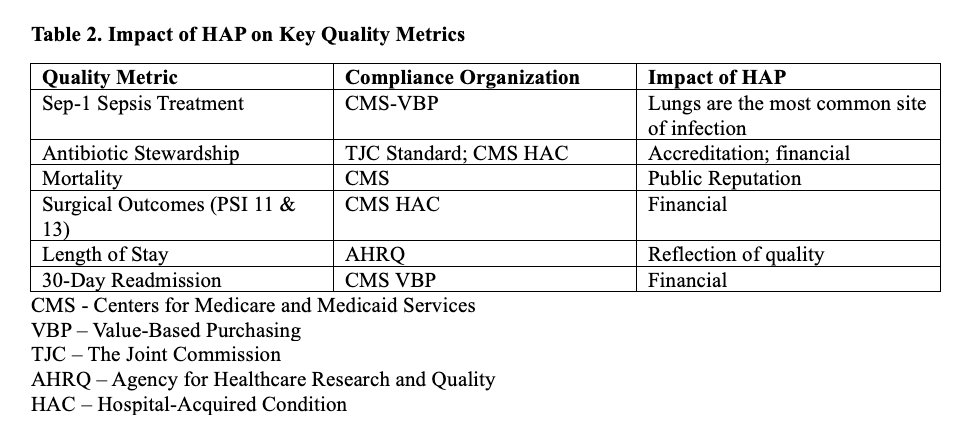
Hospital-acquired pneumonia (HAP) not only threatens patient safety but also exerts a significant financial burden on healthcare systems. According to the CDC's most recent point prevalence survey, HAP is the number one healthcare-acquired infection (HAI), accounting for one in every 4 infections.1 In addition to being highly prevalent, HAP impacts resource utilization, quality metrics, value-based purchasing (VBP) initiatives, and patient satisfaction.
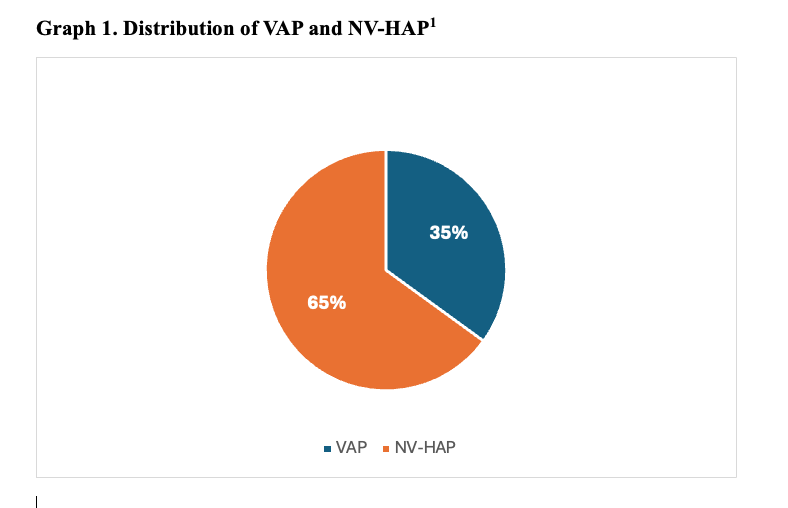
HAP is a confirmed pneumonia diagnosis that occurs 48 hours after hospitalization and is not present on admission.2 Ventilator-associated pneumonia (VAP) is associated with the use of an artificial airway, although most healthcare-acquired pneumonia (HAP) cases are not linked to a ventilator. Non ventilator-associated HAP (NV-HAP) is now a larger concern (Graph 1).
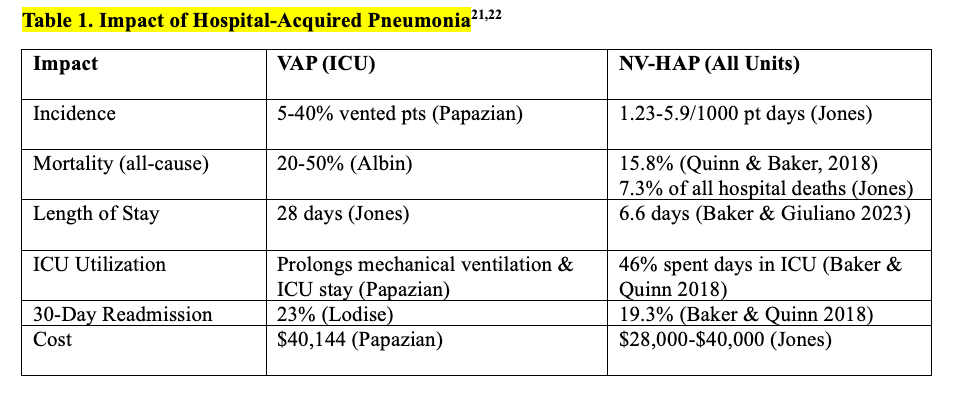
VAP and NV-HAP are frequent and serious preventable conditions that impact patients and health care systems. High mortality, increased length of hospital and intensive care unit (ICU) stays, increased utilization of ICUs, and frequent hospital readmission contribute to increased costs to patients, families, and institutions. (Table 1). In a retrospective case-control study of Medicare patients hospitalized in 2019, those with HAP were almost 3 times more likely to die within 90 days compared to matched controls without HAP, and those with HAP spent an extra week in the hospital, increasing the cost of care by 24%.3
Oral Hygiene as Prevention
While medical interventions are essential in managing HAP, oral hygiene's prevention role is often overlooked and is one of the most frequently missed elements of care.4 However, recent research underscores the hidden benefits of oral hygiene practices in averting VAP and NV-HAP, improving overall patient outcomes, including substantial cost savings and enhanced value-based care benefits.
Why use oral hygiene to prevent pneumonia? Oral hygiene is the only intervention that addresses source control by reducing the pathogens that lead to pneumonia. During hospitalization, the healthy oral microbiome is disrupted, allowing the growth and replication of pathogens that can cause infection.5 These pathogens are frequently microaspirated into the airway and can lead to pneumonia.6
Comprehensive oral hygiene breaks this chain of infection and combats pneumonia-causing pathogens before they can enter the lungs. Daily oral care is recognized as an Essential Practice in the pneumonia prevention guidelines updated in 2022.7 In a recent systematic review, daily toothbrushing was the most effective aspect of oral hygiene and was associated with a reduction in HAP, mortality, and length of stay.8
Multiple studies have shown a correlation between consistent oral hygiene and a reduction in HAP. One large urban hospital implemented a comprehensive oral hygiene program for all adult patients, including high-risk critical care and oncology. The 12-month study successfully increased oral care quality and frequency in all units and reduced NV-HAP by 39%, saving an estimated 8 lives, avoiding 500 hospital days, and saving $1.72 million in costs.9 As the implementation continued into another 12 months, oral care was incorporated into presurgical routines. Over 2 years, 164 NV-HAP cases were avoided, with an estimated 31 lives saved and $6.2 million in cost-avoidance.10
Read more in Infection Control Today HERE